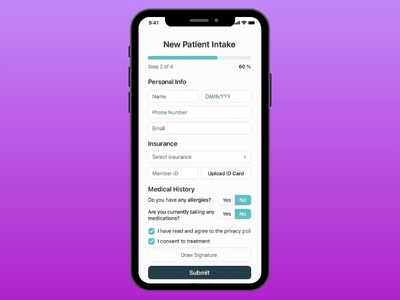
Patient-facing forms
Mobile-first, ADA-aware, multilingual, conditional logic, and e-sign.
- ID and insurance capture via camera or file upload
- Consent and attestation captured with timestamps

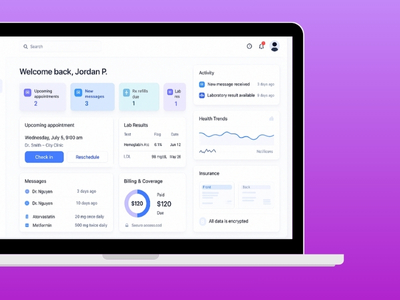
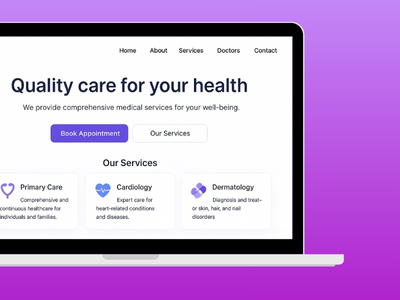
Multi-site outpatient and specialty clinics across the U.S. and Canada. The starting point was paper packets, re-keying, and fragmented portals. We delivered a digital intake layer that ops can run: mobile forms, eligibility checks, reminders, routing, and audit-ready governance.
The main issue was not “forms.” It was reliability: missing fields, missing consents, disconnected teams, and PHI travelling through too many hands.

Patients were filling long packets at the wrong time (often in the lobby), and staff were re-entering the same information across systems. That created delays, data quality issues, and avoidable privacy risk.
We built a mobile-first intake experience that can adapt by clinic, visit type, and eligibility. It routes the right information to the right team, with a full audit trail behind every step.
Mobile-first, ADA-aware, multilingual, conditional logic, and e-sign.
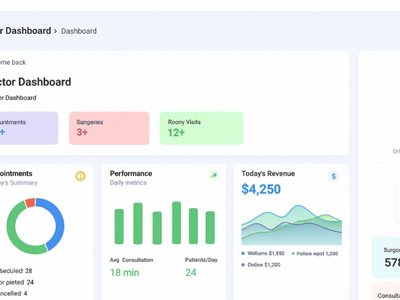
Automated checks before the visit with clear exception flags.
Two-way SMS/email within consent-aware windows.
Uploads routed to the right clinic with acknowledgements.
Ops edits questions, languages, content, and banners without code.
Time-stamped trails and exports with reason codes.
Healthcare teams do not need marketing language here. They need predictable controls: access boundaries, encryption, audit trails, and disciplined retention.

Rollout was staged clinic by clinic, with de-identified testing and clear exception handling, so operations could trust the system before expanding scope.
This is what a good intake layer changes: less typing, fewer missing items, fewer avoidable calls, and cleaner data entering downstream systems.
Note: outcomes shown are illustrative from a 12-clinic rollout and depend on workflow and change management.
